Today (6th March 2018) @NHSBenchmarking held an
event releasing the findings from their most recent round of data collection
concerning NHS/health services for people with learning disabilities. This is a
project that’s been going for a few years, where volunteer organisations (mainly
NHS Trusts) across the UK help NHS Benchmarking collect information about
health services for people with learning disabilities. I think 47 organisations
took part in 2015/16, and 49 organisations took part in 2017.
I think this project is really important, because it tries
to collect information that isn’t available in any other way (although there is
a strong case to be made that much of this information should be routinely collected
nationally). It also tries to collect information about some of the kinds of
community-based health services that the NHS England strategy Building The Right Support says are needed, if people with learning disabilities or autistic
people aren’t going to keep being unnecessarily shunted into inpatient units.
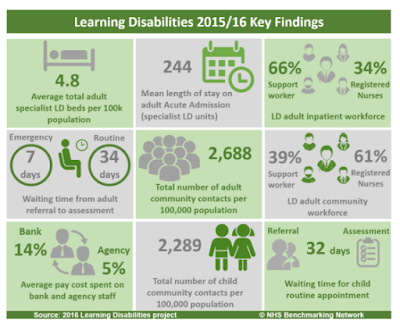
Thanks to live tweeters at the event (hashtag #NHSBNLD ) I
was able to see some of the findings from this project. NHS Benchmarking also
produced a handy summary for 2017 which you can see here, which they also produced
in exactly the same format (thank you!) for 2015/16, which I found here and is
also shown below. Although the number of organisations taking part changed from
2015/16 to 2017, some of the tweets from the event showed NHS Benchmarking
making comparisons over time so I’m assuming this is OK to do.
This post is just a quick, instant reaction to some of the
information presented today by NHS Benchmarking. I personally think it makes
pretty gloomy reading – rather than building the right community-based support,
these figures generally suggest that this support is being dismantled.
Specialist inpatient
services
The NHS England Transforming Care programme has set great
store on trying to reduce the number of people using inpatient units and
reducing the number of these units that exist. The NHS Benchmarking data (from
NHS Trusts, I think, so it doesn’t include independent sector organisations
that now run inpatient units for half of all people using them in England)
shows that the average length of stay for people in a unit has dropped slightly
from 244 days to 230 days. This includes some general mental health inpatient
units where people stay for much shorter periods of time, and can be contrasted
with the national Assuring Transformation data. For January 2018, this dataset
reported that people spent an average 987 days in their current inpatient unit,
and 1,949 days continuously in inpatient units where they had been transferred directly
between units.
More worryingly, the number of places in these units seems
if anything to be increasing. In 2015/16, there were 4.8 places in these units
per 100,000 of the general adult population – in 2017 this increased to 6.4
places per 100,000 population.
The nursing workforce in these units also changed slightly –
in 2015/16 34% of the staff were registered nurses (66% were support workers),
compared to 32% of staff in 2017 (and 68% support workers).
Across services for people with learning disabilities, in
both 2015/16 and 2017, 14% of the total pay bill was spent on Bank staff. The
percentage of the pay bill spent on agency staff increased, from 5% in 2015/16
to 7% in 2017.
Taken together, this suggests a continuing drift towards
more inpatient services, with a progressively less skilled and stable workforce
working within them.
Community teams for
adults
The NHS Benchmarking project also reported some information on
community teams for adults with learning disabilities that I don’t think is
available anywhere else.
First, the number of contacts with adults with learning
disabilities made by community health services has increased, from 2,688
contacts per 100,000 adult general population in 2015/16 to 2,756 contacts per
100,000 population in 2017. But there are signs that community health services
are ‘doing more with less’, and are creaking under the strain.
For example, the waiting time from referral to assessment
has increased for ‘routine’ referrals from 34 days in 2015/16 to 41 days in
2017. As with inpatient services, the skills of these community teams are also changing
– 61% of staff in these services were registered nurses in 2015/16, compared to
53% of staff in 2017.
Community teams for
children
The NHS Benchmarking project also reports a couple of bits
of information on community services for children with learning disabilities,
and here the trends look pretty catastrophic. In 2015/16 there were 2,289
contacts with children with learning disabilities made by community health
services per 100,000 general child population – a figure already lower than the
equivalent for adult teams. By 2017 this had dropped to 1,471 contacts with children
per 100,000 population, a drop of over a third (36%). Over the same year, the
average waiting time for a routine appointment for children with learning
disabilities increased from 32 days to 72 days.
Dismantling the right
support
The ambition and work of the NHS England Transforming Care
programme (due to finish in a year’s time), particularly in terms of building
decent community-based support services for people and families, is coming up
against the brute reality of disinvestment and cuts to exactly the types of
services specified as needed in Building The Right Support. These cuts aren’t
confined to one year either – the NHS Benchmarking report for 2016 found that
in two years from 2014 to 2016 the number of service contacts with people with
learning disabilities had dropped by 18% and the spend on these services had
dropped by 23%. These cuts seem particularly savage in services for children with
learning disabilities, which is where, if anything, support needs to be
front-loaded.
From an inadequate base, the right support is being further
dismantled.

No comments:
Post a Comment
Note: only a member of this blog may post a comment.